Florida's New Advanced Birthing Centers and C-sections
Roni Rabin, a reporter on healthcare issues for The New York Times, recently wrote about the new law in Florida allowing the establishment of “Advanced Birth Centers” which will allow c-sections to be performed in centers outside of hospitals. She notes that in Florida only two rural hospitals offer labor and delivery. The birth centers are supposed to help make obstetric services more available to women with the implication that this will help reduce maternal mortality in Florida.
There are really two problems with creating a new form of obstetrical care to help reduce maternal mortality in Florida. Much of Ms. Rabin’s article explores the problem of risk with C-sections. The second issue Ms. Rabin raises is how will these birth centers be paid.
According to Dr. Cole Greves, the Florida district chairman for the American College of Obstetricians and Gynecologists (ACOG), “A pregnant patient who is considered low risk in one moment can suddenly need lifesaving care in the next.” Yes, obstetricians know that. We’ve heard that since the first day of med school.
Dr. Greves says that these centers “cannot guarantee the level of safety patients would receive within a hospital.”
The U.S. maternal mortality rate is higher than any other developed country in the world. The U.S. rate is 23.8 deaths per 100,000 live births in 2020. In countries such as the Netherlands and Denmark, the rate is between 1 and 2 deaths per 100,000 births. With the maternal death rate what it is today in the U.S., our hospitals can’t really be considered the yardstick for quality with maternal mortality in this country.
Safety of Advanced Birth Centers Compared to Hospitals
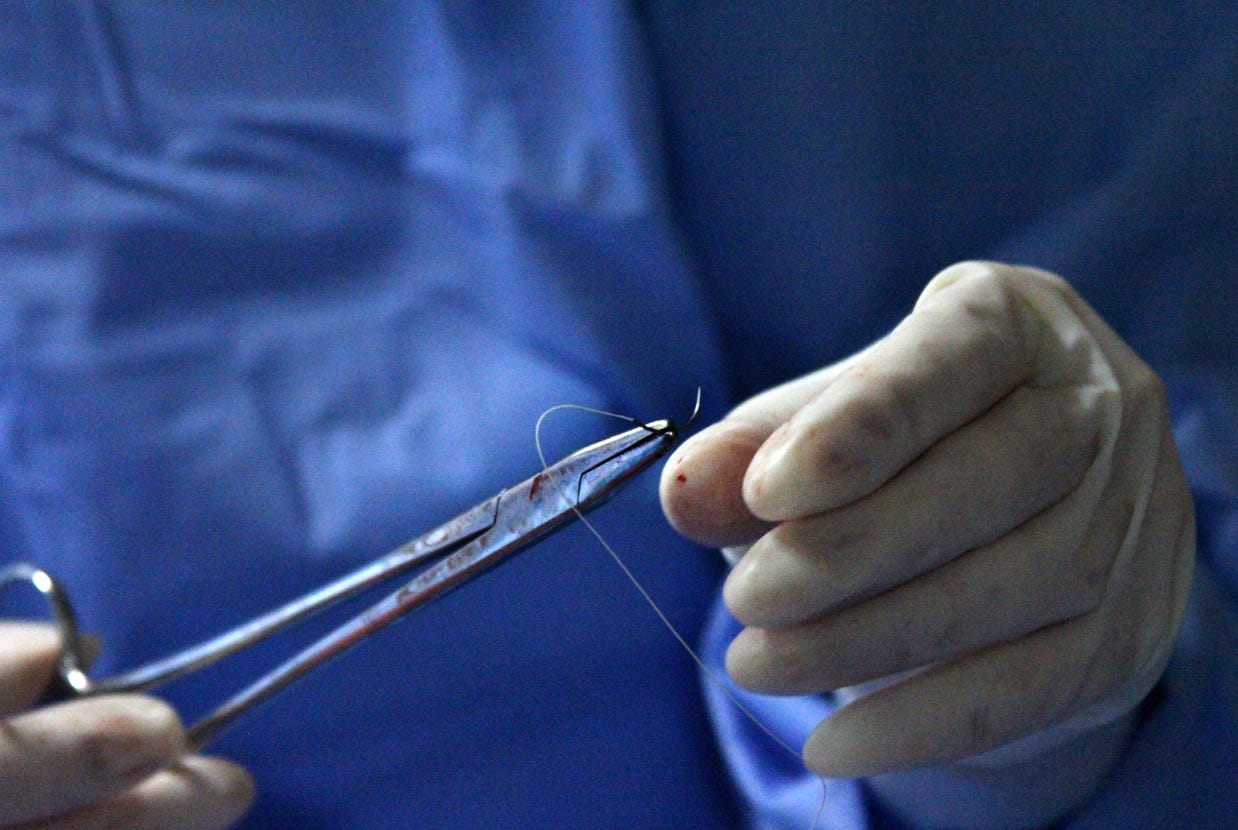
Having practiced obstetrics in rural healthcare deserts, I understand very well the idea of doing without all the bells and whistles available at large hospitals. In spite of that, I have not lost a mother’s life. One day I massaged a uterus for 8 hours to control bleeding from uterine atony, the main cause of bleeding to death from pregnancy and delivery. Fundal message is a low-tech effective way to deal with uterine bleeding. This technique would certainly be available at a Florida advanced birth center.
Incidentally, researchers are now working on an algorithm to predict who is going to have heavy bleeding. It seems to be rather pointless to say the least. Risk factors in the study include pre-eclampsia and carrying multiples. We need an algorithm to tell us this? More importantly, there is absolutely nothing subtle about postpartum hemorrhage. It is as obvious as the sun rising in the east every morning.
I struggle to imagine what would be a justifiable cause of mortality-related blood loss in pregnancy. I suppose a catastrophic automobile accident or airplane crash would be possible, but bleeding to death from delivery in a hospital should NEVER happen.
Payments to Advanced Birthing Centers a Second Problem
According to Ms. Rabin’s article, a second problem with creating advanced birthing centers is how to get paid. There is uncertainly over whether these centers will accept Medicaid patients. Furthermore, hospitals are concerned that these centers will pull their insured patients away form their labor and delivery services, causing the hospitals to lose money.
Not to rain on Florida’s parade, but I believe reimbursement is going to be their number one problem for at least the next decade. A much simpler solution, one that does not run afoul of ACOG, the Centers for Medicare and Medicaid Services (CMS), and health insurances is a specialty hospital. Most states have legislation permitting small, specialty hospitals.
For the sake of this article, I will not get into the evils of the legislation which forbids doctors from owning hospitals, but simply state that this legislation needs to be changed. Bankers are allowed to own banks, lawyers to own their own law firms, and Sam Walton to own Walmart.
Advanced Birthing Centers Will Not Reduce Maternal Mortalities
Admittedly, reducing maternal mortality is not Ms. Rubin’s subject in her article. However, the claim is made by hospitals that there is less risk in c-sections at hospitals than at advanced birthing centers. I would suggest a more effective approach to reducing maternal mortalities, as mentioned above, would be the use of specialty hospitals.
Initially, all that would be needed in a specialty hospital for prenatal care, labor and delivery, and postpartum care is an obstetrician, two state-certified midwives, and 24/7 ultrasound and anesthesia. ACOG compounds the rural desert problem by refusing to board obstetricians who see men in regular practice. One wonders why an obstetrician seeing men somehow excludes a physician from eligibility for boarding. Clearly, an obstetrician in a rural area will be unlikely be able to maintain a practice seeing only women. So what rural hospitals wind up with are visiting obstetricians a few days a month and deliveries 100 miles away. This greatly degrades the quality of obstetrical services available to rural areas and ACOG should stop preventing obstetricians from serving rural areas in order to maintain their boarding. Fortunately, the National Board of Physicians and Surgeons (NBPAS) will board obstetricians working in rural areas.
In the end, the specialty hospital would avoid the practical problems of the advanced birth center, including, but not limited to coding, insurance, both health and med-mal issues, reimbursement, and all of the other economic and political potential problems involved with advanced birth centers.
Converting High Risk Pregnancies to Low Risk Pregnancies
I certainly must agree with Dr. Greves who says, “A pregnant patient who is considered low risk in one moment can suddenly need life-saving care in the next.” We’ve all heard that from the first day of medical school. It is true. That’s why in obstetrics the concept of “high risk vs low risk” has little real meaning. Many people who have a disdain for obstetrics say that it’s 98 percent boredom and 2 percent terror. The point is that labor and delivery can go south in a hurry.
With the U.S. maternal mortality rate 36th in the world, the notion that medical care will be so much better in a hospital is difficult to support. The point of obstetrics, which many doctors and hospital administrators fail to understand, is to keep patients low risk and reduce high-risk pregnancies to low-risk pregnancies by seeing patients as often as needed and by forming a patient-provider partnership. Until the patient-physician relationship is reintroduced into the practice of obstetrics, the U.S. maternal mortality rate will not go down.
My personal preference for addressing the issue of obstetric deserts would be to establish a small specialty hospital with the option of physicians owning them.
The practice of obstetrics has changed radically over the past 30 years, and not always for the benefit of the mother, the new baby, or the family. These changes in the practice of obstetrics have been particularly hard on rural women as rural hospitals continue to close obstetrics units.
Tragically, there has been little effective effort on the part of the medical profession to work with rural hospitals to provide assistance and training to encourage rural hospitals to begin or continue offering obstetrics.
Medicine has never been a one-size-fits all discipline. Recipe medicine has never worked in medicine and it never will. The specialty hospital can form the basis of a good start in reversing the highly destructive path of the one-size-fits all strangle hold on birth and delivery in rural America.